Breast Cancer
Breast cancer is a disease that occurs as a result of a tumor that occurs due to the change and uncontrolled proliferation of one of the cell groups that make up the breast tissue.
Studies show that the incidence of breast cancer has increased considerably in recent years. According to statistics on a global scale, the incidence of breast cancer is estimated to be around 40-50 per 100000. Generally, in industrial societies, the probability of developing breast cancer in a woman's lifetime is 1/8.
Although its absence in the family is thought to be a very protective condition, 10-15% of breast cancers are familial, while 85-90% occur in women without a family history.
Despite the increase in the incidence of breast cancer, death rates due to breast cancer are gradually decreasing as a result of advances in diagnosis and treatment.
Breast Cancer Risk Factors
Since breast cancer is a common type of cancer, there are many identified risk factors. However, not having these risk factors does not mean that you will not get cancer, while the presence of risk factors does not necessarily mean that you will get cancer.
However, the probability of being caught is higher than other women who do not have these factors, and their follow-up is more important. It should be noted that half of the women with breast cancer do not have these risk factors at all.
Female gender: Being female is a risk factor in itself for this disease. Although 99% of patients are women, breast cancer can develop in 1% of men as well.
Age: It is one of the most important risk factors for the development of breast cancer. The risk of developing breast cancer increases with age. Although the majority of women diagnosed with breast cancer are over the age of 50, unfortunately, breast cancers are seen at younger ages in our country compared to western societies. Approximately 3% of all breast cancers occur in women under 35 years of age, and cancers seen in this age group generally have a worse prognosis.
Hormonal Factors (Estrogen exposure): Early menarche (first menstrual bleeding before the age of 12) and late menopause (after 55 years) cause the body to be more exposed to the hormone estrogen.
To have not given birth or to have given birth late: The fact that the first pregnancy is after the age of 35 or having never given birth to a child increases the risk of breast cancer.
Family History of Breast Cancer: 10-15% of breast cancers are familial. Especially having a history of breast cancer in a first degree relative (mother, sister, daughter, aunt, grandmother) on the mother's side is considered an important risk factor. If these members of the family are diagnosed with the disease before menopause and have bilateral breast cancer, the risk increases even more.
While the risk of developing breast cancer in a family member who does not have breast cancer is 6%, the risk of developing breast cancer in women whose relatives have had breast cancer is 11%.
If breast cancer is present in more than one close family member, if it has occurred at a young age, if the disease is bilateral or if genetic predisposition tests show such a risk, these conditions increase the risk of breast cancer and the possibility of familialism.
Two genes that have been proven to be associated with breast cancer are BRCA1 and BRCA2. Women with mutations (changes) in these genes have a much higher risk of developing breast or ovarian (ovarian) cancer than those who do not carry these mutations. In this case Hereditary Breast Cancer is mentioned.
According to him, it is very important to follow up. It is a special group different from the presence of breast cancer in the family, it is the result of a genetic defect, the probability of developing breast cancer reaches a very high rate of 50%, and a large number of breast cancer cases are encountered in the family. Hereditary breast cancer is caused by a defect in the BRCA1 and BRCA2 genes.
Hormone therapy: The use of birth control pills and the use of external hormone drugs for menopause treatment are also considered among risk factors, although it is still controversial.
Personal history of breast cancer: A woman who develops cancer in one breast has a higher risk of developing cancer in the other breast than other women in the community. In addition, ovarian, uterine and colon cancer in women also increases the risk of breast cancer. Leading benign breast diseases: Some benign breast diseases create risk factors for the development of breast cancer or increase the existing risk.
Having had a breast biopsy: The presence of a lesion in the breast that requires a biopsy is important. Moderate hyperplasia on pathological examination 1.5-2 times the risk of breast cancer (mild), atypical ductal hyperplasia 3-5 times (moderate), and lobular carcinoma in situ (without dissemination) or atypical ductal hyperplasia or lobular with family history The presence of hyperplasia increases the risk 8-10 times (highly). Patients should be followed up accordingly.
Radiation (Radiotherapy): The risk of developing breast cancer later increases in those who receive radiotherapy to the breast area at an early age, and those who are treated for lymph cancer.
This risk is especially higher in those who received radiotherapy before the age of 15. A situation that should not be confused here is to know that the radiation dose used during the imaging of the breast tissue (mammography) is so low that it does not pose a risk for the development of breast cancer, and it is not to avoid this very valuable examination for diagnosis.
Nutrition and Environmental Factors: The diet rich in fat and obesity increase the risk of breast cancer, especially in menopausal women.
The use of alcohol (regularly more than one glass a day) also increases the risk, while the effect of smoking is still debated. It is known that regular exercise and physical activity reduce the risk of breast cancer.
What Could Breast Cancer Findings Be?
Since breast cancer is the most common cancer in women, knowing its findings is particularly important.
Findings in the breast can be detected during the patient's self-examination or during the physician's examinations, but the ideal is to detect tumors much earlier during screening before any findings appear.
Findings that may be a sign of breast cancer:
• Palpable mass or lumps in the breast
• Asymmetrical changes in the breast compared to the other
• Nipple discharge
• Pulling inwards, dimples in a region of the breast
• Nipple collapse, deformity or long-lasting crusting, flaking
• Redness, swelling, non-healing wounds on the breast skin
• Palpable lumps and lumps in the armpit and swelling and edema in the same arm
• Unrepaired, especially spine hip pain
Mass in the breast:
It should not be forgotten that not every lump in the hand of the patient is cancer. They are generally benign masses, but in such a case, physician examination and necessary imaging tests are essential to distinguish the nature of this lesion.
There may be fluid-filled (cystic) or solid (solid) breast masses. Unless stated otherwise, breast cysts are considered benign, whereas solid lesions may occur from benign or malignant causes.
The masses that can be described as malignant are usually single lesions that are hard, have an irregular surface, and cannot be clearly distinguished from the surrounding tissue. Other breast cancer findings (breast deformity, skin changes, etc.) may accompany the masses.
Asymmetrical changes in the breast compared to the other breast:
Enlargement, shrinkage, shrinkage in one breast compared to the other, changes in the breast contour that is not on the other side may be a sign of breast cancer.
Nipple discharge:
Many women may have discharge, especially squeezing, at some point in their lives. However, spontaneous discharges, especially bloody discharge from one breast from one duct, may be a sign of breast cancer. They definitely need to be researched.
Pulling inwards, dimples in a region of the breast:
Inward retraction in one breast, which is absent in the other and usually developing in one region, and dimples in different positions may be a sign of breast cancer. It needs to be evaluated by a physician.
Nipple collapse, deformity or long-lasting crusting, flaking Some women's nipples are turned inward due to their breast structure. Although this situation is seen as normal, conditions such as retraction of the tip that usually involves only one nipple, non-healing crusting, scaling, and scar formation on the nipple may appear as symptoms of breast cancer.
Redness, swelling, non-healing wounds on the breast skin:
Although breast cancer mainly concerns the breast tissue, it can also manifest itself as redness, swelling and non-healing sores on the breast skin, depending on the spread to the skin or the invasion of the lymphatic channels of the skin by tumor.
Palpable lumps and lumps in the armpit and swelling and edema in the same arm:
Breast cancers usually spread through lymph channels. In breast cancer, swelling and lump formation in the armpit can be seen, usually accompanying breast findings, and sometimes without any detectable symptoms in the breast. In more advanced cases, swelling and redness involving the same arm may accompany this condition. Detailed investigations are essential.
Unrepaired, especially spine hip pain:
Breast cancer can metastasize to bones, especially in advanced cases. In this case, bone pain can be severe. Unfortunately, sometimes the tumor in the breast may appear unnoticed only while these pains are being investigated.
Breast Cancer Types
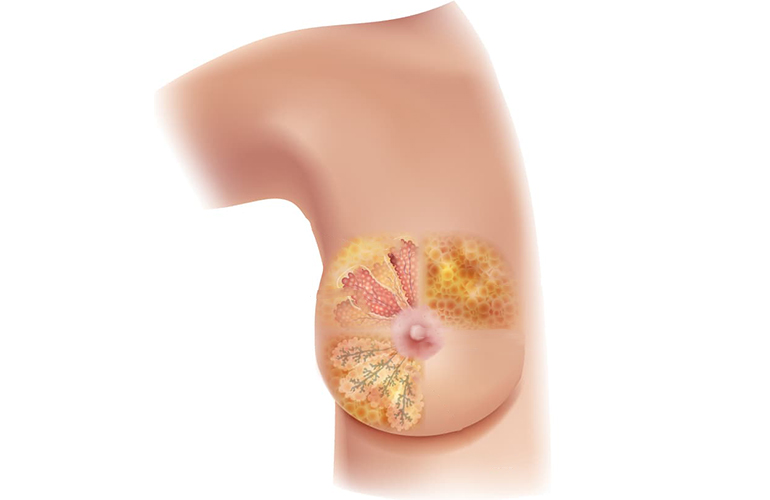
Breast cancers can be divided according to their potential to spread and also by type of histology.
According to the spread potential, the basic classification is noninvasive or in situ (not spreading), invasive (having the potential to spread) group.
Ductal carcinoma, which develops in the cells lining the breast ducts that carry milk out of the nipple, is the most common type of breast cancer. Ductal carcinoma is known to be in situ form if it does not spread, and in invasive form if it has the potential to spread.
From the milk-producing glands (lobule)
cancer that develops is called lobular carcinoma. Lobular carcinoma is also divided into two according to its spread. If it has the potential to spread in the in situ form if it does not spread, it will be in the invasive form.
Noninvasive Cancers
With the technological advancement and the prominence of screening mammograms, the rate of detection of non-invasive cancers in earlier cases (from 1.4 percent to 10 percent) and therefore the incidence among all breast cancers (from 5 percent to 15 percent) has increased. Cancers that do not spread (in situ) are again divided into two groups according to tissue type as 'ductal carcinoma in situ' and 'lobular carcinoma in situ'.
Classic lobular carcinoma in situ: Detection of its presence increases the risk of breast cancer 8-10 times in both breasts. In the treatment, in addition to close monitoring, some protective drugs such as anti-estrogen tamoxifen can be given. In appropriate cases, removal of both breast tissues (simple mastectomy) and prosthesis and similar surgical reconstructive procedures with plastic surgery interventions can be applied as a preventive measure.
Ductal carcinoma in situ (DCIS, intraductal cancer): It occurs as irregular small areas of calcification and/or (pleomorphic microcalcification) bloody, transparent single duct nipple discharge, which are often not detected on examination and observed on mammography. DCIS is considered as a step in the transformation into cancer cells with the potential to spread (invasive). Since it usually does not form a palpable mass, it can be removed by marking with wire or radioactive materials.
If the cancer is in a single focus, enough clean tissue can be left around it. When radiotherapy (RT) is applied to the remaining breast tissue, the disease shows a good clinical course. If imaging and pathological findings show that it is widespread in the breast, all breast tissue should be removed (simple mastectomy), and in this case, up to 100 percent complete recovery is observed.
Since the involvement of axillary lymph nodes is very rare in DCIS, patients who will have the entire breast removed; In some types with more aggressive features (high grade, etc.), it may be necessary to remove the first guard lymph nodes (sentinel lymph node biopsy) where the lymph channels are emptied due to the involvement of cancer cells in the armpit lymph nodes.
Invasive Cancers
It means that the tumor has crossed the base layer on which the cells sit. It is named according to the tissue in which it develops. Invasive ductal carcinoma, which develops in the cells of the walls of the milk ducts, is the most common type of breast cancer. Cancers that develop from the milk-producing glands (lobules) are called lobular carcinomas. If this has the potential to spread, they are called invasive lobular carcinoma.
Inflammatory breast cancer is a special type of breast cancer with the worst and fastest course. Unfortunately, the clinical picture can be confused with inflammatory diseases of the breast. It progresses with widespread redness and hardness without showing any signs of mass. In inflammatory diseases of the breast that do not heal despite antibiotic treatment, breast cancer should be considered and a biopsy should be taken.
Hereditary Breast Cancer
BRCA1 and BRCA2 genes are two genes involved in the repair of damage to cell DNA. If mutations in the BRCA1 and BRCA2 genes develop, the risk of developing breast cancer increases because DNA repair is impaired. Defective genes are passed on to family members, and people who carry the damaged gene may have a very high risk of developing breast cancer, such as 85-90% (whole lifetime risk of developing breast cancer is 87%).
Breast cancer usually occurs in more than one first-degree relative (mother, sister or daughter) and usually (65%) develops in both breasts. In women in this group, 70% of breast cancer occurs before the age of 45.
Genetic counseling should never be forgotten in the event that more than one person among family members has breast cancer, individuals with breast cancer are at a young age, and individuals develop cancer in both breasts.
Tamoxifen can be used for prophylaxis to manage the risks of BRCA1 Gene carriers. However, for this drug to be effective, the presence of receptors with appropriate junction points is required, and unfortunately, tumors that develop in this case usually do not contain these receptors. For this reason, there are limitations in terms of its usefulness. In cancers developing in those carrying the damaged BRCA2 gene, the use of tamoxifen reduces the risk of developing breast cancer and its use is recommended since these receptors are generally seen as positive.
In women with BRCA1 and BRCA2 gene mutations, emptying both breasts can be considered as a preventive measure to reduce the risk of cancer development. Prostheses can be placed in place of breast tissue. Since all of the breast tissue cannot be removed even in such interventions, 10% of breast cancer can be seen in these women.
In addition, ovarian cancer risk is high (50%) in damaged BRCA1 carriers.
It is recommended that the umbilical cords be purchased when the fertility work is completed.
Breast Cancer Treatments
Surgical Treatments
Breast Conserving Surgery
The main purpose of treatment is to treat breast cancer without causing organ loss. For this reason, it is accepted as the standard treatment for stage I-II breast cancer today, but it is important to stay on the target of clearing the tumor tissue and saving the patient's life.
In the surgery, the tumor part is removed with adequate clean surgical margins. Since breast tissue remains in the patient after breast-conserving surgery, the patient must be told that the patient must receive radiotherapy for the remaining tissue. This treatment cannot be applied to patients who cannot receive radiotherapy for any reason. Sometimes, if the tumor is large in proportion to the breast, breast-conserving surgery may not give the patient the desired result cosmetically.
In women with large breasts, it is possible to get both breast cancer and reduce both breasts to ideal sizes at the same time. With this method, besides the surgical treatment of cancer, the patients experience problems due to large breasts (breast pain, backache, shoulder pain, limitation of movement, rash that does not go away under the breast, spinal curvature, difficulty in radiotherapy, etc.) are saved.
Mastectomy
Mastectomy is the complete removal of breast tissue. Today, it is applied for patients with large-scale and/or widely distributed (multifocal) tumors in the breast where breast-conserving surgery is not suitable or in cases where the patient does not accept it. It is the classical surgical treatment method of breast cancer. Provides good local control; The risk of recurrence of the tumor is low.
If breast cancer is hereditary in some patients with a family history of breast cancer in first degree relatives, mastectomy can also be performed on the disease-free breast for risk-reducing and protection purposes.
It can also be performed in the form of 'nipple-sparing mastectomy' in early-stage tumors, skin-sparing or tumors located far from the nipple.
During the surgery in which the nipple is preserved, a single dose of radiotherapy (intraoperative radiotherapy) can be given to the patient's nipple while under anesthesia and on the operating table.
In the presence of genetic mutation, mastectomy option can be applied to reduce the risk. It is possible to obtain good aesthetic results with different reconstruction methods in all breast surgeries.
Underarm Control
The purpose of the procedures (sentinel lymph node sampling, axillary lymph node dissection) to understand whether the axillary lymph nodes are tumorous or not, is to accurately stage the disease and guide concomitant treatments, and if lymph involvement is detected, to provide regional tumor control.
The presence or absence of armpit (axillary) lymph node involvement is one of the most important parameters regarding the course of breast cancer (to what extent it threatens the patient's life).
Sentinel Lymph Node Biopsy
Breast cancers tend to spread through lymph channels. Knowing the condition of the axillary lymph nodes is important in diagnosis, treatment, and follow-up, as cancer cells usually go to the axillary lymph nodes first. For this purpose, a method to evaluate the first (guard) lymph node where the lymphatic flow is drained has been developed. This approach is based on the very low probability of bypassing this place and metastasizing to other lymph nodes.
Removal of axillary lymph nodes is necessary for tumors that have spread (invasive). In-situ cancers do not theoretically need to be cleaned under the armpit, as they do not go to the lymph nodes. In the procedure, a special dye is injected into the area of the tumor or under the nipple, alone or together with a radioactive substance.
In order to find the lymph nodes where the lymph channels are empty, a direct armpit incision is made and only the stained lymph nodes are removed. During the surgery, pathological examinations are performed, and if they contain a tumor, the remaining part of the lymph nodes in the armpit is removed. If no tumor cells are seen, the process is terminated.
Axillary Lymph Node Dissection
Removal of underarm lymph nodes is called axillary lymph node dissection. Studies conducted in recent years have shown that in this procedure, 8-10 lymph nodes must be removed in order for the armpit to be sampled correctly.
This process provides better local area control. However, the procedure may have complications such as swelling in the arm (lymphedema), fluid accumulation in that area (seroma), temporary limitation of movement. For this reason, some precautions such as protecting the patient's hand and arm from injuries and exercises should be taken.
Non-surgical treatments
Radiotherapy
Radiotherapy (Radiation therapy) is a form of treatment using X-rays and is applied to provide local control of the tumor. Radiotherapy is used before or after surgery, as a curative treatment alone or in combination with chemotherapy/systemic treatment.
If breast-conserving surgery is preferred, radiotherapy to the remaining breast tissue is absolutely necessary. If a mastectomy (removal of the entire breast) was performed, the radiot the need for therapy depends on some requirements (For example: the tumor is attached to the chest wall or breast skin, there are more than 4 positive lymph nodes under the armpit, etc.)
Ideally, radiotherapy should be administered within 6 months following breast surgery. If chemotherapy is being administered at this time, either it is expected to end or radiotherapy can be given by interrupting chemotherapy.
In patients whose axillary lymph nodes have been removed after radiotherapy, the risk of swelling in the arm (lymphedema) increases if radiotherapy is required to this area. Pregnant women are not recommended to receive radiotherapy because of the risk of harming the unborn baby.
In a very limited patient group, radiotherapy can be applied only around the tumor instead of the entire breast, the procedure can be performed during or after surgery (intraoperative radiotherapy).
Chemotherapy
The drug treatment used to stop the growth and spread of cancer cells or to destroy the spread is called chemotherapy. Surgery and radiotherapy provide local treatment of breast cancer, while chemotherapy and hormone therapy aim at systemic treatment. Chemotherapy of breast cancer is still one of the most researched subjects in the world.
Chemotherapy is an adjuvant approach to surgical treatment in many patients, but in some cases (for example, in disseminated disease) it takes on the role of primary treatment. Adjuvant chemotherapy after surgical treatment of breast cancer reduces the risk of recurrence of breast cancer and increases survival.
Chemotherapy called neoadjuvant can be given before surgery to provide preoperative control in advanced cases or to make it suitable for surgical treatment in unsuitable cases. Chemotherapy is often used in the 2nd-3rd day after the operation. starts a week. Problems with wound healing may delay chemotherapy.
One or more combinations of drugs can be used. Depending on the time planning, there may be 4, 6 or 8 cycles. Chemotherapy can suppress the bone marrow and negatively affect the body's defense system. Special side effects may occur due to drugs.
Hormonotherapy
If the tumors of the patients are sensitive to estrogen and/or progesterone hormones (if their tumors carry hormone receptors), hormone drugs (hormonotherapy) that are structurally similar to these hormones but with suppressive properties are given. For this purpose, the most widely used anti-estrogen agent today is tamoxifen.
In recent years, other agents with similar efficacy have been developed besides tamoxifen (such as aromatase inhibitors). Tamoxifen can also be used for prevention in patients at high risk for developing breast cancer. For this purpose, the period of use is 5 years and they reduce the risk by 40-50% on average only during the period of use.
Tamoxifen may cause symptoms similar to menopause in the early period. Long-term use has been associated with uterine cancer. For this reason, the duration of use in women in the premenopausal period is limited to 5 years. Aromatase inhibitors given after menopause have some side effects such as osteoporosis and joint pain.
Targeted Therapy (Smart Medicines)
Cancer treatments such as chemotherapy and radiotherapy also affect healthy cells without separating healthy cells from cancer cells. targeted therapies; It is designed to destroy only cancer cells, reduce damage to healthy cells and minimize side effects that negatively affect the patient's quality of life.
With antibodies and smart molecules that act directly on the cancerous cell, the side effects of chemotherapy are tried to be reduced in the treatment. Cancer cells in about one in five women with breast cancer have a cancer-promoting receptor protein known as HER-2 on their surface (HER2; human epidermal growth factor receptor 2).
HER2-positive breast cancers tend to grow and spread more aggressively. In these patients, chemotherapy and hormonal treatments alone may be insufficient. When smart drugs such as “Herceptin, Tykerb, Perjeta” developed to silence these receptors are given together, they increase the effect of chemotherapy and hormonal therapy.

